As mentioned above, unfortunately the visual field segments that were lost due to glaucoma cannot be re-instated. However, given that glaucoma is a progressive disease, it should be treated as soon as it is diagnosed in order to prevent further deterioration and loss of vision.
Glaucoma treatment is primarily aimed at reducing the pressure in the eye and this can be achieved with medication, the use of laser or surgery.
Medication
Fortunately, the medication that is currently being used to for glaucoma is very effective in controlling intraocular pressure, and most patients are regulated with the daily use of one or more eye drops, once or twice a day.
The mechanism of action differs depending on the medication category, so they can be administered in combination, achieving even greater reduction in intraocular pressure.
Like all medicines, eye drops too have specific indications, contraindications and side effects which means they must be used by patients with consistency and responsibly.
Although this medication is topically administered to the eye, they are rapidly absorbed from the circulation and they also have a systemic effects, potentially affecting all organs of the human body. The doctor always takes into account other health problems that may exist (heart failure, asthma, etc.) in order to prescribe a safe and effective treatment.
Treating Glaucoma with Laser
Despite the great efficacy of anti-glaucoma medications, sometimes these do not suffice in reducing intraocular pressure while other times there may be application or compliance issues by the patient himself.
In these cases, several Laser techniques can be used, which ultimately increase the drainage of aqueous humor from the eye.
In chronic simple glaucoma (open angle glaucoma) the Laser acts directly on the drainage angle, bringing about structural changes that increase its effectiveness.
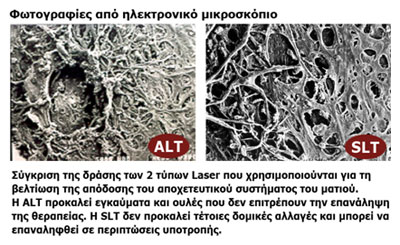
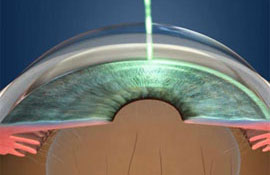 Apart from the traditional and widespread Argon Laser Trabelucoplasty (ALT), in recent years Selective Laser Trabeculoplasty (SLT), which has the advantage of not disturbing the tissues into the drainage system of the eye and can be repeated in cases of recurrence, has successfully been used.
Apart from the traditional and widespread Argon Laser Trabelucoplasty (ALT), in recent years Selective Laser Trabeculoplasty (SLT), which has the advantage of not disturbing the tissues into the drainage system of the eye and can be repeated in cases of recurrence, has successfully been used.
 In acute glaucoma (where the angle is closed) a special Laser is used to open a hole in the iris from where the aqueous humor will discharge, resulting in an immediate decrease in pressure.
In acute glaucoma (where the angle is closed) a special Laser is used to open a hole in the iris from where the aqueous humor will discharge, resulting in an immediate decrease in pressure.
Surgically treating glaucoma
If, despite the medication or use of laser the pressure has not been satisfactory regulated and there is still a risk of optic nerve deterioration, the ophthalmologist can begin examining other choices that are performed in the operating room.
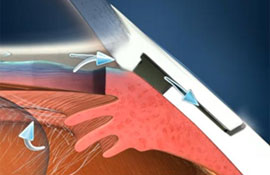 Traditional glaucoma surgery are performed under local anesthesia and aim at creating a new permanent channel for the discharge of the aqueous humor. A successful "trabeculectomy" (same name as the surgery) is characterized by the creation of a bubble/blister ("filtration ampule") at the upper segment of the eye where the fluid is temporarily being retained before being absorbed by the surrounding blood vessels. Although it is the most widespread of all the anti-glaucoma interventions, complications are not rare and in some cases can be very serious.
Traditional glaucoma surgery are performed under local anesthesia and aim at creating a new permanent channel for the discharge of the aqueous humor. A successful "trabeculectomy" (same name as the surgery) is characterized by the creation of a bubble/blister ("filtration ampule") at the upper segment of the eye where the fluid is temporarily being retained before being absorbed by the surrounding blood vessels. Although it is the most widespread of all the anti-glaucoma interventions, complications are not rare and in some cases can be very serious.
 In recent years the implantation of artificial valve mechanisms from various materials such as silicone has gained significant ground, having the added advantage of controlling the outflow of aqueous humor in order to avoid excessive discharge phenomena and to achieve more stable levels of intraocular pressure.
In recent years the implantation of artificial valve mechanisms from various materials such as silicone has gained significant ground, having the added advantage of controlling the outflow of aqueous humor in order to avoid excessive discharge phenomena and to achieve more stable levels of intraocular pressure.
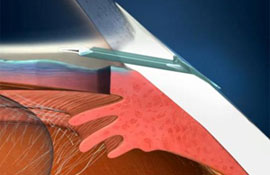
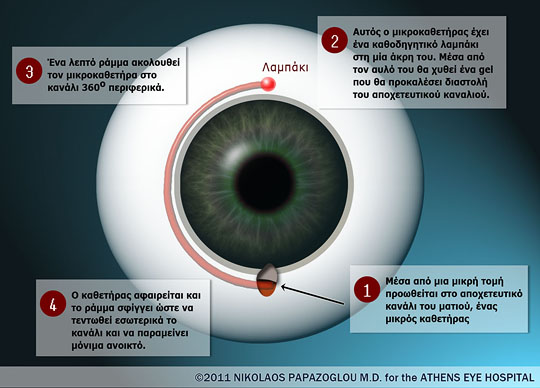
A new promising technique for opening the drainage channels of the eye is "canaloplasty". With this method, a new aqueous humor discharge channel is not opened as in previous operations, but rather attempts are made to restore and improve the existing, natural drainage mechanism available to the human eye.
In this method (which is reminiscent of the vascular surgeons opening arteries with balloons) is performed by making a very small incision, via which a small catheter is inserted that is promoted as the main drainage channel of the eye, in the region of the iris. Material in the form of a gel is then injected into the drainage channel resulting in its dilation. A thin suture follows the microcatheter in the circular path through the channel, which is tightened after removal of the catheter to stretch the channel and keep it permanently open.
Do you use eye drops for glaucoma or another eye disease? Are you sure that you are using it properly?
Very often after a visit to the ophthalmologist we end up with a prescription for one or more eye medications in the form of drops or ointments.
One of the most misunderstood practices in ophthalmology and perhaps throughout medicine is the manner with which drops should be applied to the eye.
The drops do not have the capacity to penetrate the skin so it is futile to hope that we are taking our medication simply by applying the medication around the eye or on the eyelashes.
For the medication contained in the drops to take effect, it must be placed inside the pouch (like a pocket) which the lower lid forms in order to be absorbed by the blood vessels.
If you use more than one eye drop and their administration time coincide, it is advisable to wait 5-10 minutes before administering the next eye drop. Conversely, the immediate application of one after the other "flushes" the previous one before it has had time to be absorbed.
It is pointless to administer more than 1-2 drops because the eye has the capacity of approximately one droplet. Hence, if you administer 10 drops for example, only one will remain in the eye and the other 9 will run off onto your cheek like tears. Given the high price of some eye drops, this is not only non-beneficial, but also uneconomical.
 German
German Ελληνικά
Ελληνικά