Visual stimuli are recruited from the retina, where they are converted into nerve impulses in order to finally reach the occipital lobe of the brain at the back of our head, for recognition and processing.
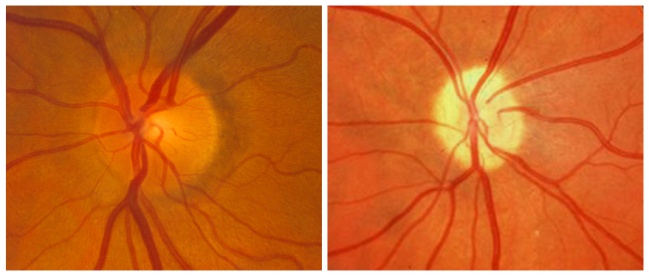
The transfer of nerve impulses from the retina to the brain is via the optical path, of which the first part is the optic nerve. The start of the optic nerve is visible during pupilloscopy (an examination with special lenses where we can observe the interior of the eye) and appears as a pale hollow discoid formation known as the optic disc.
Optic nerve hypoplasia
If the development of the optic nerve does not reach completion by the time of birth, an optic disc appears - pale and smaller in size than normal. Depending on the degree of hypoplasia, the effects on vision range from minor to very serious
The disease may involve one eye or both and remains stable over time, i.e. neither worsens nor improves. As the optic nerve is a continuation of the brain, it is not uncommon to coexist with other neurological disorders as well as pituitary hypoplasia - a very important gland that regulates many functions of our body including growth.
Therefore, children with hypoplasia of the optic nerve should undergo a detailed imaging and hormonal examination, as any failure of the pituitary gland can disrupt a child's development.
Atrophy of the optic nerve
While hypoplasia of the optic nerve refers to the incomplete development of the nerve during pregnancy, atrophy is the result of an underlying cause such as a brain tumour or a serious injury to the child's head. Symptoms include a reduction of central and peripheral vision as well as impaired colour perception.
If the cause that led to atrophy is not obvious, a detailed examination should be made to exclude conditions that can be life-threatening for the child.
Papilloedema
Sometimes the optic disc of one or both of the child's eyes may show - during a pupilloscopy performed by an ophthalmologist - an exuberant, edematous image and a vagueness to its boundaries.
The first thing that needs clarification is whether this a real papilloedema or rather some anatomical variation inherited from the child’s parents. The consideration of parents’ pupils usually gives the answer, especially in a child exhibiting no headaches or reduced eyesight.
True papilledema may be caused by brain tumors, subarachnoid hemorrhage, hypothyroidism, and various drugs, such as an overdose of vitamin A, quinolones and tetracyclines.
 German
German Ελληνικά
Ελληνικά