If we consider the eye (in an oversimplified way) as a ball, then its wall comprises of three layers: the retina in the inside, the uvea in the middle and the sclera in the front.
The uvea consists of the iris and the ciliary body in the anterior, and the choroid in the posterior.
Anterior uveitis (iridocyclitis)
Iridocyclitises are often idiopathic, i.e. their exact cause is not always found, while they can accompany other ophthalmic or systematic causes.
The anterior uveitis can occur after an injury or surgical procedure, while a quite common cause is herpes infections of the eye, including herpes zoster.
A laboratory examination for the histocompatibility antigen B27 (HLA-B27) is quite often positive.
Systematic diseases, such as seronegative arthritis (ankylosing spondylitis, psoriatic arthritis etc), tuberculosis, syphilis and sarcoidosis may cause iridocyclitis.
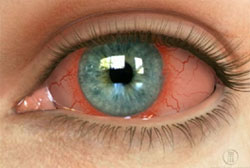 The symptoms include photophobia, pain deteriorating through reading, lacrimation and redness that can be more intense around the cornea. The constriction of the pupil’s sphincter causes its contraction (miosis), while in serious cases, the inflammatory elements accumulate at the lower part of the anterior chamber forming hypopyon.
The symptoms include photophobia, pain deteriorating through reading, lacrimation and redness that can be more intense around the cornea. The constriction of the pupil’s sphincter causes its contraction (miosis), while in serious cases, the inflammatory elements accumulate at the lower part of the anterior chamber forming hypopyon.
Iridocyclitic diseases can be acute or chronic, unilateral or bilateral, and, quite often, they relapse.
Most of the cases respond well to treatment with local steroids and mydriatic eye drops. If the disease becomes more serious, complications, such as glaucoma, cataract and macular edema, may appear.
Posterior uveitis
It is an inflammation of the choroid, that is, the posterior part of the uvea. As the anterior uveitis, it may be an isolated disorder or part of a multi-systematic disease.
Symptoms include floaters and blurry vision (caused by the inflammatory elements in the vitreous, namely, the gel inside the eye). Usually, there is neither pain nor redness at the external of the eye.
A series of tests, such as fluoroangiography, laboratory blood screening and chest X-rays, must be carried out, in order to determine the exact cause.
Treatment depends on the cause, but it usually includes the use of local or systematic steroids.
Intermediate uveitis
It characteristically affects teenagers and young adults, with floaters and vision clouding in one or/ and both eyes. It is of unknown aetiology and is also treated with steroids.
Masquerade syndromes
They are mostly serious ophthalmic disorders, which are clinically presented as anterior or posterior uveitis, without being primarily inflammatory.
They include retinoblastoma, leukemia, lymphoma, malign melanoma, retinal detachment etc.
The basic problem with these disorders is that, as they are initially taken as uveitis, they lead to wrong treatment and delay of the proper one, resulting in increased ophthalmic morbidity and a life threatening condition of the patient.
 German
German Ελληνικά
Ελληνικά